Whether it be two physicians trying to change shifts or an assistant trying to change the department on-call schedule, communicating these changes to the hospital can be lengthy. Through traditional channels such as faxes, or post-it notes, mistakes can easily be made and information overlooked.
Current Scheduling Reality: What a Pain!
Let’s look at a realistic hospital situation. Sheryl works at the on-call desk. She is responsible for taking all the department calls when a shift change is made throughout the hospital. Say the emergency department contacts Sheryl to change two on-call physicians. Sheryl takes out her whiteout, updates the on-call schedule and then loads it into the fax, sending it to all the departments, phone operators and the countless other entities involved. This happens several times a day and Sheryl receives these changes through various channels including phone, email, and of course, fax.
Meanwhile, Nancy, one of the many administrative assistants, starts off her day taping the hospital on-call schedule to her desk for easy access. She receives countless faxes during the day, mostly from Sheryl, and she doesn’t have the time or the manpower to update it accordingly every time. So what does she do? She sets out 2 time slots during her day to collect the faxes and update the schedule. How long is the schedule inaccurate? How often is the information shared incorrect?
As the article The slow disappearance of the fax machine in healthcare on the HealthIT Exchange points out:
“In addition to security concerns, traditional fax machines can be inefficient and unreliable.”
Is it Nancy’s or Sheryl’s fault? Of course not. However, everybody pays the price of an inaccurate process.
At the department level, when two physicians switch shifts, Nancy needs to update the changes to Sheryl, who then needs to take out her whiteout, again, and fax it back to her programmed contacts throughout the hospital.
Why Do Hospitals Still Use Outdated Technologies?
Despite the many innovative options available to physicians and hospitals, some health organizations seem hesitant to change their ways. Faxes are still widely used and administrators and phone operators skim through folders and paperwork to find the right information. Because of the lack of efficiency of these methods, they often do not have an updated version of what they are looking for and costly mistakes occur.
The Ponemon Institute’s study on The Economic and Productivity Impact of IT Security on Healthcare highlights that:
“An average of more than 45 minutes each day [is wasted] due to the use of outdated communications technologies.”
The scheduling challenges that hospitals face, even in 2015, are indeed linked to outdated systems and methods. Some hospitals even hire additional personnel whose main purpose is to manage various department schedule changes.
Some of these scheduling challenges include:
- vacations and holidays
- shift preferences
- communicating changes
- seniority
- staff coming and going
- hospital staff requirements
With the current tight hospital budgets and priorities shifting to ensure patient care is not affected by these cuts, most do not have the resources for such personnel. Managing physician absences is a job on its own without technology. Is there not a better way?
Time to Increase Hospital Performance
Hospitals are increasingly looking into adopting technology to increase performance and decrease costs. Scheduling software contributes to hospital-wide coordination and provides the right information to all personnel, at all times.
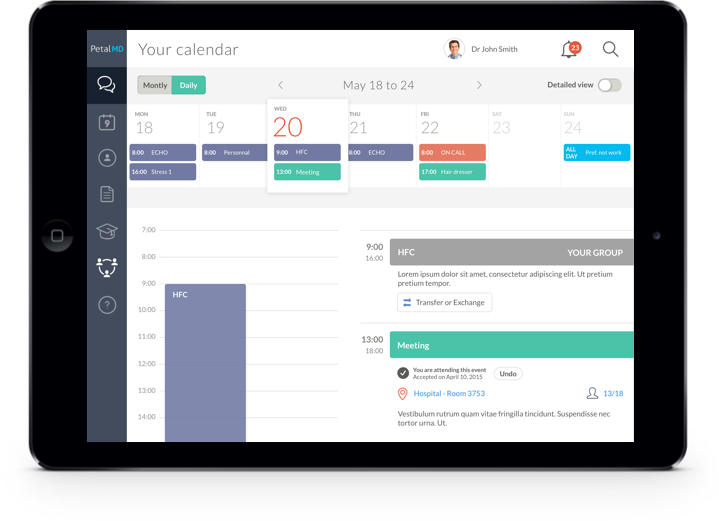
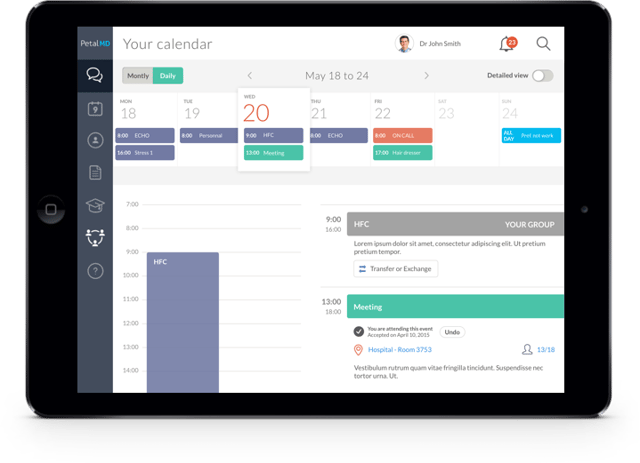 PetalMD’s hospital-wide on-call schedule solution provides the hospital staff important information, all in real-time and on any device. The web-based platform requires no installation and also provides physicians access to secure messaging.
PetalMD’s hospital-wide on-call schedule solution provides the hospital staff important information, all in real-time and on any device. The web-based platform requires no installation and also provides physicians access to secure messaging.
